Hydrea
Hydrea
- In our pharmacy, you can buy hydrea without a prescription, with delivery in 5–14 days throughout the United Kingdom. Discreet and anonymous packaging.
- Hydrea is intended for the treatment of chronic myeloid leukaemia, sickle cell disease, and various myeloproliferative neoplasms. The drug acts as an antimetabolite chemotherapy agent, inhibiting DNA synthesis.
- The usual dose of hydrea for adults is 20-30 mg/kg once daily for chronic myeloid leukaemia and 15-20 mg/kg for sickle cell disease.
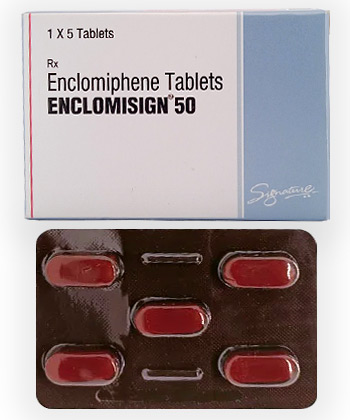
- The form of administration is a capsule.
- The effect of the medication begins within 24 hours.
- The duration of action is approximately 24 hours, depending on the dosage and individual response.
- Do not consume alcohol while taking hydrea.
- The most common side effect is neutropenia.
- Would you like to try hydrea without a prescription?
Hydrea
Basic Hydrea Information
- International Nonproprietary Name (INN): Hydroxyurea
- Brand names available in United Kingdom: Hydrea
- ATC Code: L01XX05
- Forms & dosages: Capsules (500 mg)
- Manufacturers in United Kingdom: Bristol Myers Squibb, Meda AB
- Registration status in United Kingdom: Prescription-only (Rx)
- OTC / Rx classification: Prescription-only
Everyday Use & Best Practices
When it comes to taking Hydrea, timing is a key factor, but the choice between morning and evening dosing often depends on personal routines and preferences. Many patients prefer a morning schedule as it integrates seamlessly into their daily routine, often alongside breakfast. However, evening doses may be more convenient for those who have busy mornings, allowing flexibility. This adaptability can help maintain a consistent medication regimen, reducing the likelihood of missed doses and fostering adherence to treatment plans.
Taking With or Without Meals (UK Diet Habits)
One common question is whether to take Hydrea with food. In the UK, patients typically have regular meal patterns, with breakfast around 7-9 am, lunch from 12-2 pm, and dinner from 6-8 pm. Taking Hydrea with food can help mitigate any potential stomach upset, which some individuals may experience. While it is not mandatory to take Hydrea with meals, doing so aligns with the common UK dietary habits. Patients should consider their own meal timing and preferences when integrating the medication into their routine.
Ultimately, ensuring that Hydrea is taken consistently—whether with or without food—can significantly impact medication adherence. Recognising the key role that dietary habits play in medication scheduling is crucial for patient management and overall health outcomes. Remain aware of how food interactions might influence side effects and consult healthcare professionals for personalised advice on the best practices for taking Hydrea.
What’s Inside & How It Works
Ingredients overview
Hydrea’s main active ingredient is hydroxyurea, a vital component in its formulation that acts as an antimetabolite. This means it interferes with the growth and replication of cancerous or abnormal cells. In addition to hydroxyurea, the capsules may contain excipients—these are inactive ingredients that help with formulation and stability. Common excipients could include starch, gelatin, or magnesium stearate, which aid in the manufacturing process and ensure that the medicine is effective and safe for consumption.
Mechanism basics explained simply
Hydrea works by reducing the amount of DNA in cells, which inhibits the growth of abnormal blood cells. In conditions like sickle cell disease, this medication helps to increase the production of fetal haemoglobin, replacing the sickle-shaped cells with healthier red blood cells. For chronic myeloid leukaemia (CML), hydroxyurea slows the proliferation of cancer cells, thus managing the disease effectively. By targeting these mechanisms in straightforward terms, patients can understand how the medication aids in reducing symptoms and improving their overall condition.
Main Indications
Approved uses (MHRA listing)
In the UK, Hydrea is primarily prescribed for several medical conditions. These include:
- Sickle cell disease
- Chronic myeloid leukaemia (CML)
- Polycythemia vera
- Essential thrombocythemia
These indications are recognised by authoritative sources like the Medicines and Healthcare products Regulatory Agency (MHRA), ensuring safe and effective use. Patients can trust that these uses have undergone rigorous testing and approval processes.
Off-label uses in UK clinics
In addition to the approved indications, Hydrea is often used off-label for other conditions, such as acute leukaemia or solid tumours in some clinical settings. While making these decisions, healthcare professionals exercise clinical discretion, evaluating potential benefits versus risks carefully. Such practices emphasise the need for tailored treatments based on individual patient needs and circumstances.
Interaction Warnings
Food interactions (alcohol, tea/coffee)
Patients taking Hydrea should be cautious with their diet, particularly when it comes to alcohol and caffeine. Alcohol can exacerbate the side effects of Hydrea, such as gastrointestinal discomfort and drowsiness, further impacting the patient’s wellbeing. Similarly, excessive consumption of tea or coffee may interfere with the medication's effectiveness. It's advisable to discuss any dietary concerns with a healthcare provider to ensure optimal management while on Hydrea.
Drug conflicts (MHRA Yellow Card reports)
There are notable drug interactions to be aware of while using Hydrea. For instance, concurrent use of other myelosuppressive agents (drugs that suppress bone marrow activity) like certain chemotherapy agents can increase the risk of severe side effects, including increased vulnerability to infections or bleeding. Additionally, interaction with medications that affect liver enzymes can alter hydroxyurea metabolism, requiring careful monitoring. Patients should always inform their healthcare teams about all medications they are taking to avoid complications.
Latest Evidence & Insights
Recent studies conducted between 2022 and 2025 have offered new insights into the efficacy and safety of Hydrea. Findings indicate that long-term use of hydroxyurea not only manages symptoms effectively but also improves patients' quality of life by reducing occurrences of crises in sickle cell disease. New research points to potential applications in treating other blood disorders, showcasing Hydrea's versatility. Such advances in understanding the drug’s role within chemotherapy cycles are significant for evolving treatment methodologies in the UK.
Alternative Choices
For those seeking alternatives to Hydrea, several options are available through NHS prescribing. Here’s a quick comparison:
- Ruxolitinib (Jakavi): Effective for myeloproliferative neoplasms, yet comes with a higher risk of infections.
- Anagrelide: Specifically targets platelets, but potential cardiovascular side effects may limit its use.
- Interferon-alpha: Used for CML, known for its immune-modulating effects; however, it can cause flu-like symptoms.
- Luspatercept: Promising for beta-thalassemia and sickle cell, though still under evaluation.
Each alternative has its pros and cons, and healthcare providers should evaluate the expected outcomes and possible side effects with patients. Understanding these nuances ensures the right choice tailored to individual health needs.
Regulation Snapshot
The regulation of Hydrea (hydroxyurea) in the UK falls under the jurisdiction of the Medicines and Healthcare products Regulatory Agency (MHRA). This approval is crucial for ensuring that the medication is safe and effective for use in various conditions, including sickle cell disease and certain myeloproliferative neoplasms. Professionals are guided by the NHS prescribing framework, which outlines specific indications for prescribing Hydrea. Clinicians must assess the risks and benefits for each patient, taking into consideration factors such as prior therapies and the patient's overall health status. It's essential for prescribers to monitor patients regularly for side effects and treatment efficacy to ensure optimal outcomes.
FAQ Section
Many patients have common concerns about Hydrea.
What are the possible side effects? Hydrea can cause side effects, including:
- Hematological issues such as neutropenia, anemia, and thrombocytopenia.
- Gastrointestinal symptoms like nausea, vomiting, and diarrhoea.
- Dermatological reactions including skin ulceration and changes in pigmentation.
Are there any interactions I should be aware of? Hydrea may interact with other medications, particularly those affecting bone marrow function.
What should I do if I miss a dose? If a dose is missed, take it as soon as you remember, unless it’s close to the next scheduled dose. Never double up to catch up.
Consult with a healthcare professional for personalised advice on Hydrea and how it fits into individual treatment plans. Regular check-ups will also help manage any potential side effects effectively.
Guidelines for Proper Use
UK pharmacist counselling style
When patients are prescribed Hydrea, a pharmacist typically engages them in a supportive and informative manner. Key conversation points include:
- Explaining how to take Hydrea, stressing the importance of adherence to the prescribed regimen.
- Discussing potential side effects and urging patients to report any unusual symptoms immediately.
- Emphasising the need for regular blood tests to monitor blood counts and adjust the dosage if necessary.
This interaction aims to equip patients with knowledge, fostering a sense of empowerment in managing their treatment.
NHS patient support advice
Patients receiving treatment with Hydrea should be aware of additional support services available through the NHS.
Resources include:
- Regular monitoring for side effects and treatment effectiveness through recall appointments.
- Access to patient support groups for those dealing with similar conditions, fostering community and shared experiences.
- Contact details for healthcare professionals, ensuring patients can get support when needed.
It's vital to know that help is available, and reaching out for support can significantly enhance the treatment journey.
Delivery Information
| City | Region | Delivery Time |
|---|---|---|
| London | Greater London | 5-7 days |
| Birmingham | West Midlands | 5-7 days |
| Manchester | Greater Manchester | 5-7 days |
| Glasgow | Scotland | 5-7 days |
| Leeds | West Yorkshire | 5-7 days |
| Newcastle upon Tyne | Tyne and Wear | 5-7 days |
| Sheffield | South Yorkshire | 5-7 days |
| Bristol | South West England | 5-7 days |
| Cardiff | Wales | 5-7 days |
| Nottingham | East Midlands | 5-9 days |
| Southampton | South East England | 5-9 days |
| Leicester | East Midlands | 5-9 days |
| Brighton | South East England | 5-9 days |
| Coventry | West Midlands | 5-9 days |
| Stoke-on-Trent | Staffordshire | 5-9 days |